Home to the largest population of grizzly bears and bison in the continental United States, Montana hosts some of the most striking North American wilderness in large, wild swaths. According to a research from Colorado College in 2013 and 2014, 63% of Montanans hunt and/or fish, 60% camp, and another 57% hike. Perhaps these numbers explain the 73% of Montanans who identify themselves as conservationists. This strong environmental ethos is intertwined in the economy, which centers on industries such as agriculture, mining and energy, tourism, and healthcare.
The state’s iconic landscapes in Yellowstone or Glacier National Parks, ranches, historic mountain towns, and legendary ski resorts draw visitors seeking outdoor adventure. However, these natural treasures coexist along challenges including mining-related pollution, climate threats, and rural health access that impact children in particular.
Recently, Montana released up to $3.7 million of funding to help replace old diesel vehicles with electric, alternate fuel, or newer diesel models to reduce NOx emissions. In 2024, the state also started to fund projects that will build the electrical grid system’s ability to withstand extreme events and natural hazards. In the profile below, you’ll find a set of key children’s environmental health indicators that illuminate Montana’s environmental risks, children’s exposures, and emerging trends in child health and development.

Safe Drinking Water:
31.7% of public water utilities had drinking water violations in 2023.
National average: 27.6%

Air Quality:
62.14% of children under age 18 live in counties with unhealthy levels of air pollution. Air quality was monitored in 12 out of 56 counties in Montana in 2024.
Nationwide: 39.88% of children

Warming Temperatures:
4.1 degrees F warmer in 2024 than in 1970.
National average 3.9 degrees F warmer

Toxic Chemical Releases:
52 million pounds of toxic chemicals were disposed of or released in 2023.
United States 3.3 billion pounds
Asthma:
7.5% of children under age 18 have asthma (2022-2023).
Nationwide: 6.6%

Pediatric Cancer:
162 cases of pediatric cancer per 1 million population (2021).
Nationwide: 179 cases per 1 million
Blood Lead Levels:
There is insufficient data available to calculate the percentage of children with elevated blood lead levels in the state.
Neurodevelopmental Disorders:
14.7% of children age 3-17 have ADHD (2022-2023).
Nationwide: 10.5%
3.2% of children age 3-17 have Autism Spectrum Disorder (2022-2023).
Nationwide: 3.9%
Children’s environmental health indicators (CEHIs) are measures that can be used to assess the magnitude or extent of environmental hazards, environmental exposures, or children’s health outcomes.
Each headline indicator should be a clear, understandable indicator of children’s environmental health, with broad relevance for a range of audiences at the state level – with relevance to the national level.
The indicators as a package should provide a representative picture of children’s health and relation to the environment.
Each indicator should be calculated using an agreed-upon (and published) method and accessible and verifiable data.
Each indicator should be calculated regularly (at least biennially), with a short lag between the end of the period and publication of the data.
The available data needed for the indicator must be sufficiently robust, reliable and valid.
Indicators must be comparable across all or very nearly all 50 U.S. states.
KIDS COUNT Data Book: State Trends in Child Well-Being. The Annie E. Casey Foundation. Accessed April 2025.
In this profile, counties with “unhealthy” levels of air pollution are those receiving a grade of F for ozone and/or short-term particle pollution (PM2.5), and/or a grade of “Fail” for year-round particle pollution (PM2.5) in the American Lung Association’s 2024 State of the Air report. According to the report, 62.14% of Montana children under age 18 live in counties that received a failing grade for at least one pollutant. This only considers the 12 counties where air quality data is monitored, collected, and sufficient (out of 56). Across the US, 39.88% of children under the age of 18 live in counties with unhealthy levels of at least one measure of air pollution. Nationwide, air quality data is monitored, collected, and sufficient in 885 counties (out of 3,243 total).
2024 State of the Air Report. American Lung Association. Accessed April 2025.
Children are more vulnerable to the hazards driven by warming temperatures, such as heatwaves, droughts, flooding, and many other cascading effects. Climate change causes an increase in the frequency and severity of temperature anomalies, extreme weather, and natural disasters globally.
EPA’s Toxics Release Inventory (TRI) tracks the management of certain toxic chemicals
that may threaten human health and the environment. Industrial facilities across the
U.S. are required to annually report the amount of each chemical disposed of or
released into the environment, both on- and off-site. Many of these chemicals are
known carcinogens, developmental toxicants, and neurotoxicants that adversely impact
children’s health, such as arsenic, lead, and mercury.
A wealth of research links exposure to poor outdoor air quality, including high concentrations of ground-level ozone, with the exacerbation of children’s respiratory illnesses, including asthma. Several studies link it with the onset of childhood asthma.
2022-2023 National Survey of Children’s Health. Title V Maternal and Child Health Services Block Grant National Performance and Outcome Measures. Prevalence of current asthma, age 0-17 years. Data Resource Center for Child and Adolescent Health. Maternal and Child Health Bureau, Health Resources and Services Administration. Accessed April 2025.
Although cancer in children is rare, the rate of pediatric cancer has been increasing since the 1970s. It is the leading disease-related cause of death past infancy in U.S. children. Neither genetics nor improved diagnostic techniques can explain the increased rate. According to the 2020 Childhood Cancer Prevention report, no more than 10% of all childhood cancers are derived from heritable genetic risk factors, and hazardous chemicals are a preventable risk factor that contributes to the remaining cases.
Insufficient data was available for blood lead levels in Montana children. There is no safe level of lead exposure for children. A potent neurotoxicant, lead reduces IQ and impairs other cognitive, behavioral, and developmental functions. In 2021, the CDC lowered the BLL reference value from 5 to 3.5 μg/dL, but much of the available data still categorizes “elevated” BLLs as being 5 ug/dL or higher.
No reports or data found for Blood Lead Level Indicator.
Assessing Child Lead Poisoning Case Ascertainment in the US, 1999–2010. Eric M. Roberts, Daniel Madrigal, Jhaqueline Valle, Galatea King and Linda Kite. Pediatrics April 2017, e20164266; DOI: https://doi.org/10.1542/peds.2016-4266.
Mounting scientific research links environmental exposures with risk of Attention-Deficit Hyperactivity Disorder (ADHD) and Autism Spectrum Disorder (ASD). Neither genetics nor changing diagnoses or other artifacts fully account for the increased incidences of these conditions. ADHD and ASD data are for children aged 3-17 years in this state.
2022-23 National Survey of Children’s Health. Title V Maternal and Child Health Services Block Grant National Performance and Outcome Measures. Prevalence of current ADHD, age 3-17 years; and Prevalence of current Autism or Autism Spectrum Disorder (ASD), age 3-17 years. Data Resource Center for Child and Adolescent Health. Maternal and Child Health Bureau, Health Resources and Services Administration. Accessed April 2025.
NIEHS/EPA Children’s Environmental Health and Disease Prevention Research Centers. 2017 Impact Report.
Indicator references often link to sites and data that are not managed by CEHN. Federal websites, especially, may no longer be available. Each time we release an updated factsheet, please be assured that we will also update relevant indicator references to reflect any changes.
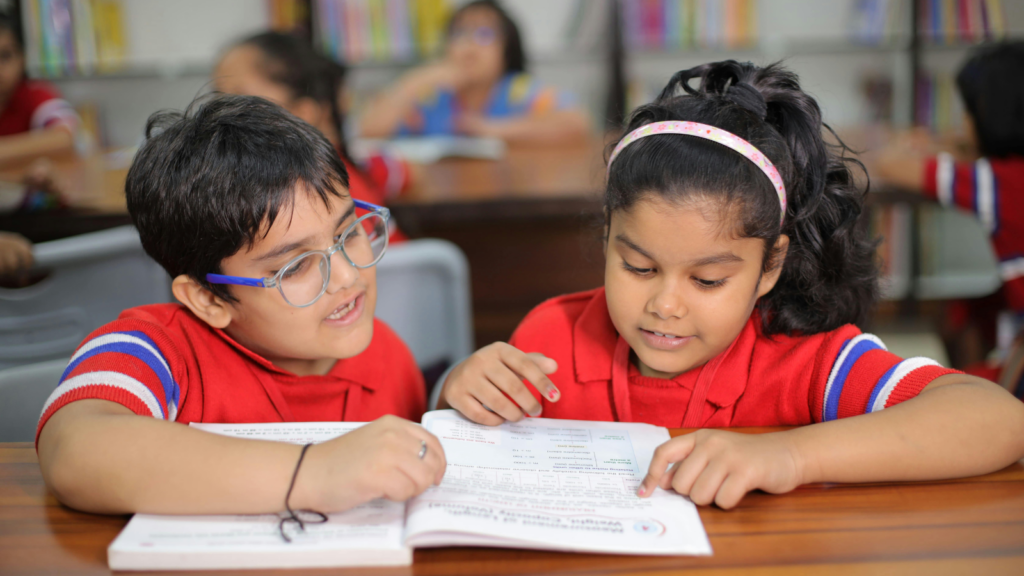
All children deserve and need a safe and healthy environment to grow and develop. They need clean air to breathe, safe water to drink, nutritious food to eat, and healthy places in which to live, learn, and play. Early exposure to harmful agents can lead to acute and chronic adverse outcomes. Infants and children are especially vulnerable to environmental exposures because they breathe, eat and drink more, in proportion to their body size, than do adults, and because their bodies and brains are still developing.
A blueprint for Protecting Children’s Environmental Health Network set out to identify a set of CEHIs that can be used to provide an understanding of children’s environmental health at the state level. Through this process, CEHN found that robust, valid, and regularly updated state level data–that are comparable across most states–were not readily accessible. States need adequate funding and capacity to collect and make accessible reliable CEHI data in order to set goals and track progress towards improving children’s health.
Children are our future – society has a moral obligation to protect them. Exposure to environmental hazards can and must be prevented. Prevention requires strong environmental regulations, fully funded and supportive public and environmental health programs and a robust workforce.